Value-Based Healthcare: A new model of care management
Health Care Systems in the long term across the globe is under pressure due to the increases in demand for care and the increases in the costs of providing such assistance. These pressures on the system have shifted the focus from a medicine based on volumes to a medicine that focuses on effectiveness and outcomes. There is no international forum or congress nowadays that doesn’t talk about Value-Based Healthcare as one of the necessary changes to guarantee the sustainability of Health Systems and to improve citizens’ quality of life. However, this shift represents a complete model change that is not fast or easy, and requires structural and cultural changes.
Why is it necessary to turnaround Healthcare Systems?
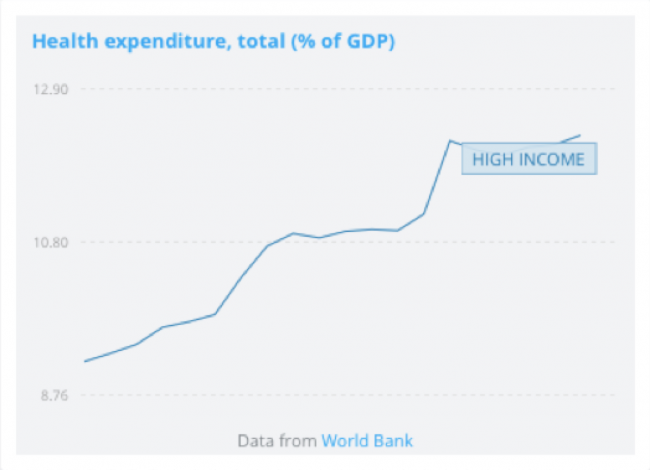
The sustainability in the mid/long term of the Health Systems in developed countries has been questioned repeatedly over the last years. According to data from the World Bank, in 1995 healthcare expenditure represented already 9.2% of the GDP of OECD countries. By 2015 it already represented 12.3% of GDP(1). The situation is especially alarming if we take into account that structural factors that are affecting both the supply and the demand for health services, are pointing to a significant increase in health expenditure in the mid/long term.
On the demand side, the demographic changes, as well as the increase of the prevalence of chronic diseases and the changes of expectations of citizens are increasing the Healthcare bills. The progressive proportion of population over the age of 65 (which for countries like Spain is expected to represent 35% of the total population by 2050) will lead to an important increase in the prevalence of the chronic diseases. It is widely acknowledged that 70% to 80% of all healthcare costs in EU countries are spent on treatments of chronic diseases. The increase in life expectancy will therefore also increase the prevalence of chronic conditions, putting further pressures on the sustainability of the healthcare systems. Furthermore, citizens are becoming increasingly demanding with the system, as they want to have a more active role in the care of their health and have higher expectations of the quality of care they receive.
On the supply side, healthcare providers, both public and private, are also experiencing an increase in the cost of providing care. Both the Pharma and the Health Tech sectors have achieved great innovations in recent decades, but this has also increased the costs of providing care significantly. Surgeries are made with newer techniques and better equipment, but are also becoming more and more expensive every day. New drugs, therapies and prosthetics are also increasingly the overall costs. In Spain it is estimated that medical technologies are responsible for 33% to 50% of the increase in health expenditure (4).
All this reasons leave Health Systems across the globe under a serious problem of sustainability that cannot be solved unless important structural changes are conducted. The new paradigm requires a broader focus, with new variables of action that include, among other changes, a greater focus on the management of population health and preventive medicine, comprehensive care and continuity of care.
What is ‘Value-Based Healthcare’?
Some countries have already started wide transformations in their Healthcare Systems in order to face the above-mentioned sustainability problems. Within those trends, one of the most relevant is the shift towards Value-Based Health Care, in which care is measured based on the value that it generates for the citizens instead of the volumes and number of services and procedures provided. The Value-Based Health Care concept, also known by its acronym VBHC, was first coined by Porter, Teisberg, Kaplan, Bohmer and Christensen and the basic theory is explained by Porter, Nobel Prize in Economics, in his famous book ‘Redifining Healthcare (2006)’ and in the article ‘What is value in healthcare?’ published in the New England Journal of Medicine in 2010.
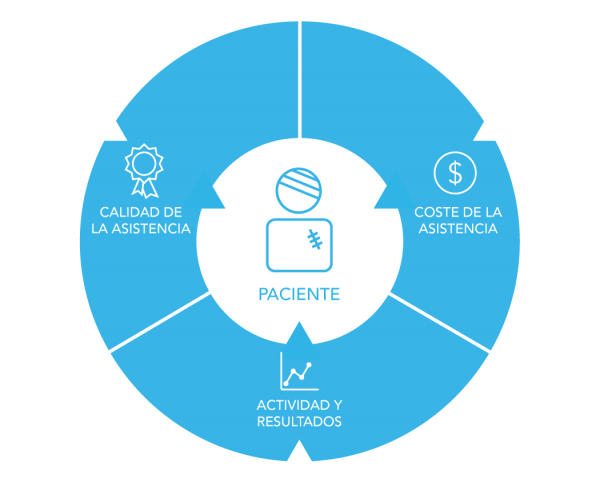
The theory of Value-Based Health Care is suggests a change of model in which the provision of health services doesn’t focus on the quantity of services provided but on the value they generate, understanding value as overall quality of care and health outcomes related to the costs achieving those outcomes(3).
Following this theory, other frameworks and theories that qualify and modify the initial VBHC model have been developed by governments and experts, but the underlying concept for all of them is the same: a change of focus towards a medicine based on results, efficiency and value generation.
The implementation of this new model will have important positive consequences for all the stakeholders of the sector:
- For the patients, shifting to a VBHC model means safer, more appropriate and effective care, with better health results and quality of life.
- For care providers, the new model implies using evidence-based medicine and proven treatments and techniques that take into consideration patient’s preferences.
- For the entire society, the new model means having a more efficient and sustainable health system.
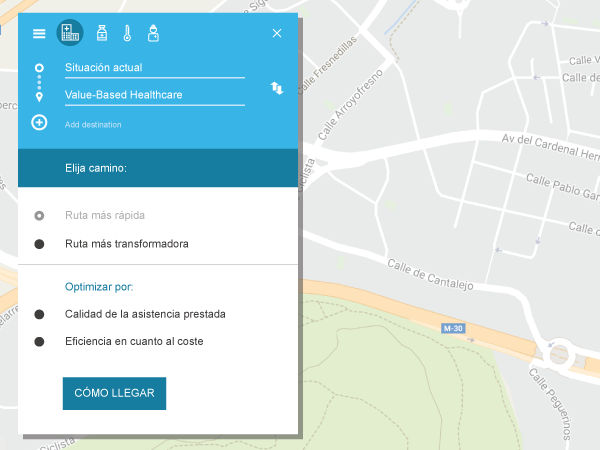
Roadmap towards Value-Based Health Care
Even though few experts challenge the validity and benefits of the theoretical model and the need to implement it, the path required to do so is complex and requires a profound transformation at many levels.
Numerous national and international institutions are identifying and piloting some structural measures that could serve as roadmap to reach a system based on VBHC. The Institute for Strategy & Competitiveness; Competitiveness at Harvard Business School, one of the most advanced agents in the promotion and investigation of Value-Based Health Care, identifies seven key pillars as the path towards achieving a medicine based on value generation (7). Those pillars range from a reorganization of the care services to the implementation and promotion of the use of adequate information systems.
Entre los pasos necesarios para poder llegar a sistema de VBHC, cabe destacar la importancia que todos los expertos dan a la implementación de sistemas que permitan la medición de la calidad y el coste real de la asistencia. Si no se implementan sistemas que permitan recoger, objetivar y cuantificar la actividad, no se podrá medir y mejorar la eficiencia y los resultados en salud.
La medición de la calidad y la eficiencia de un Servicio de Salud es una tarea difícil por su complejidad intrínseca. La dificultad radica principalmente en que la calidad asistencial es un atributo subjetivo y relativo y el coste real de la asistencia prestada es complejo de medir con exactitud. Pese a dicha complejidad, existen hoy en día sistemas e indicadores aceptados internacionalmente y con base científica probada, que permiten objetivar la información y realizar este tipo de análisis y comparaciones.
Varios organismos internacionales están trabajando ya en la definición más exacta de procesos, estándares e indicadores universales de calidad en la práctica clínica que permitan una medición aún más precisa y global de la calidad de la asistencia. Sin embargo, la mayoría de los expertos opinan que a día de hoy, existen indicadores suficientemente exactos como para que las instituciones puedan medir y evaluar la calidad y los costes reales y que estas deben implementar cuanto antes sistemas informáticos robustos que les permitan llevar a cabo dichas mediciones y análisis.
A la hora de implementar nuevos sistemas, es importante tener en cuenta que no es suficiente con la simple implantación de los mismos. Es esencial también promover e incentivar su uso en todos los estamentos de la Organización Sanitaria. Actualmente ya existe en muchas instituciones información suficiente para realizar una gestión sanitaria basada en criterios objetivos, pero nos encontramos en muchas ocasiones con que esta información no es utilizada adecuadamente y se siguen utilizando mayoritariamente criterios no-objetivos para la gestión. Asegurar que, además de sistemas de información adecuados, existe una cultura dentro de las organizaciones de análisis de la información y gestión basada en evidencia, es una de las claves esenciales para una implantación efectiva del modelo VBHC.
Para más información sobre sistemas de medición de la actividad, el coste y la calidad asistencial, ponte en contacto con nosotros.
FUENTES
- “Health expenditure, total (% of GDP).” Health expenditure, total (% of GDP) | Data, Health expenditure
- EUROSTAT. Population projections 2004-2050. Luxemburgo: EUROSTAT; 2005.
- REFLECTION PROCESS on CHRONIC DISEASES. European Commission, REFLECTION PROCESS on CHRONIC DISEASES .
- “Las claves de la Sostenibilidad del Sistema Sanitario.” Deusto Business School, Las claves de la Sostenibilidad del Sistema Sanitario.
- “Institute For Strategy & Competitiveness.” Value-Based Health Care Delivery – Institute For Strategy And Competitiveness – Harvard Business School, Value-Based Health Care Delivery.